Managing the Flare-Ups
Understanding Autoimmune Skin Conditions
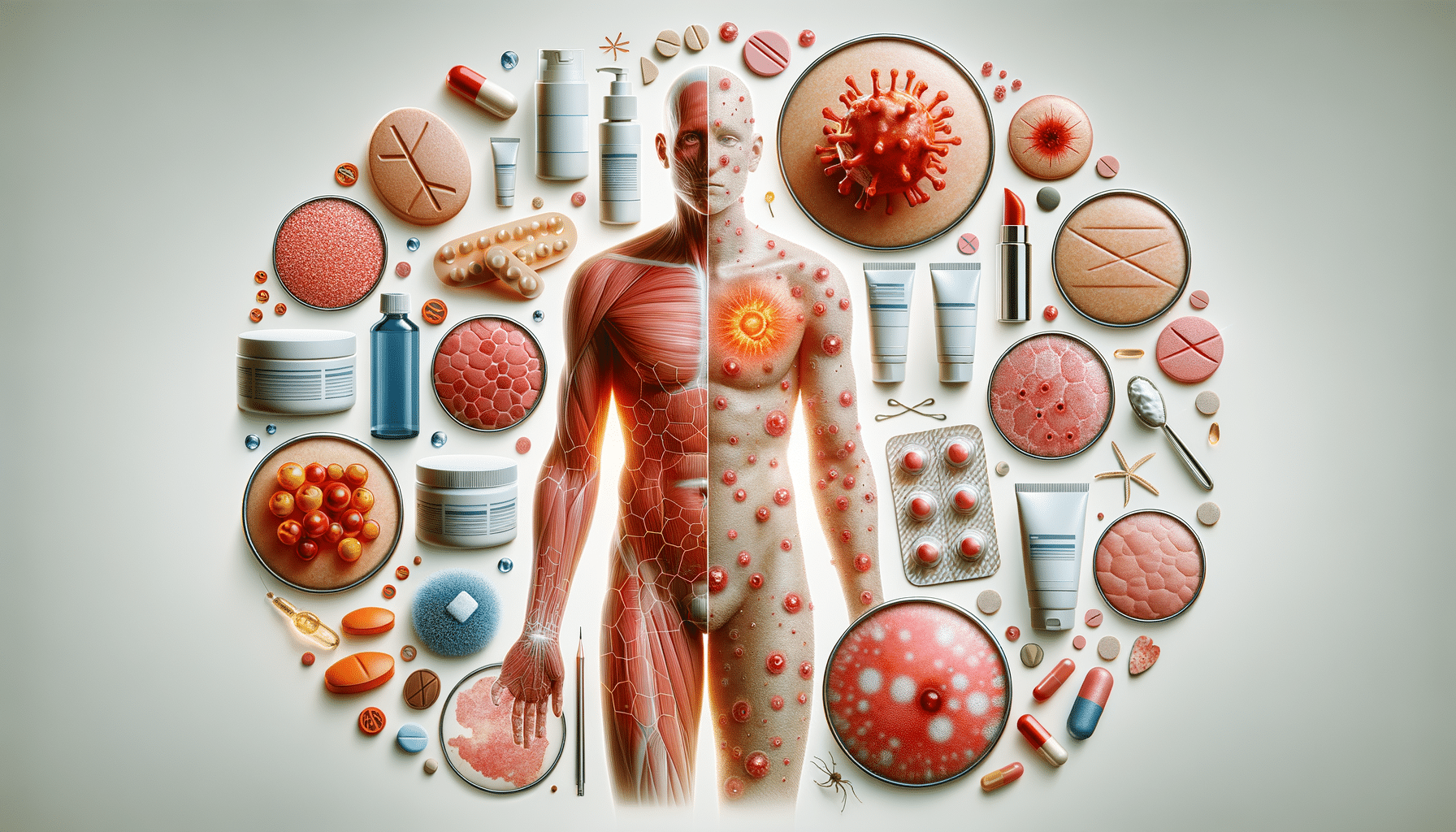
Autoimmune skin conditions are a subset of disorders where the body’s immune system mistakenly attacks its own skin cells. This can lead to a variety of symptoms, including rashes, blisters, and lesions. These conditions are often chronic, meaning they persist over time and can significantly impact a person’s quality of life. Notable examples include psoriasis, lupus, and vitiligo. Each of these conditions has unique characteristics, but they all share the common trait of the immune system’s misguided attack on healthy skin.
The complexity of autoimmune skin conditions lies in their unpredictable nature. Flare-ups can occur without warning, triggered by factors such as stress, infections, or even changes in weather. This unpredictability makes management challenging and requires a comprehensive understanding of the condition. Patients often find themselves navigating a cycle of remission and flare-ups, which can be both physically and emotionally draining.
Symptoms and Diagnosis
Symptoms of autoimmune skin conditions can vary widely depending on the specific disorder. Common symptoms include redness, swelling, itching, and the formation of scales or blisters. For instance, psoriasis is characterized by red patches with silvery scales, while lupus may present with a butterfly-shaped rash across the cheeks and nose. Vitiligo, on the other hand, involves the loss of skin pigment, leading to white patches.
Diagnosis of these conditions typically involves a combination of physical examination, medical history, and diagnostic tests. Dermatologists may perform skin biopsies or blood tests to rule out other conditions and confirm a diagnosis. Early diagnosis is crucial, as it allows for more effective management of the condition and can help prevent severe flare-ups.
Treatment Options
Treatment for autoimmune skin conditions often involves a combination of medication and lifestyle changes. Topical treatments, such as corticosteroids, are commonly used to reduce inflammation and relieve symptoms. In more severe cases, systemic medications that affect the entire body, such as immunosuppressants or biologics, may be prescribed.
Beyond medication, lifestyle adjustments play a critical role in managing these conditions. Patients are often advised to avoid known triggers, maintain a healthy diet, and manage stress effectively. Regular follow-ups with healthcare providers are essential to monitor the condition and adjust treatment plans as necessary.
Living with Autoimmune Skin Conditions
Living with an autoimmune skin condition requires a proactive approach to health and wellness. It’s important for patients to educate themselves about their condition and engage in open communication with their healthcare providers. Support groups and counseling can also be valuable resources, providing emotional support and practical advice from others who share similar experiences.
Individuals can benefit from developing a personalized skincare routine that accommodates their specific needs. This might include gentle cleansing, moisturizing to prevent dryness, and using sun protection to avoid triggering flare-ups. Additionally, some patients find relief through complementary therapies such as acupuncture or meditation, which can help reduce stress and improve overall well-being.
Future Directions in Research and Treatment
Research into autoimmune skin conditions is ongoing, with scientists exploring new treatments and potential cures. Advances in genetic research and biotechnology are paving the way for more targeted therapies that could offer greater efficacy with fewer side effects. Personalized medicine, which tailors treatment to an individual’s genetic makeup, holds promise for more effective management of these complex conditions.
Emerging treatments, such as biologics, are already making a significant impact by targeting specific pathways involved in the immune response. As research continues, there is hope for even more innovative solutions that could transform the lives of those affected by autoimmune skin conditions.