Managing the Flare-Ups
Introduction to Autoimmune Skin Conditions
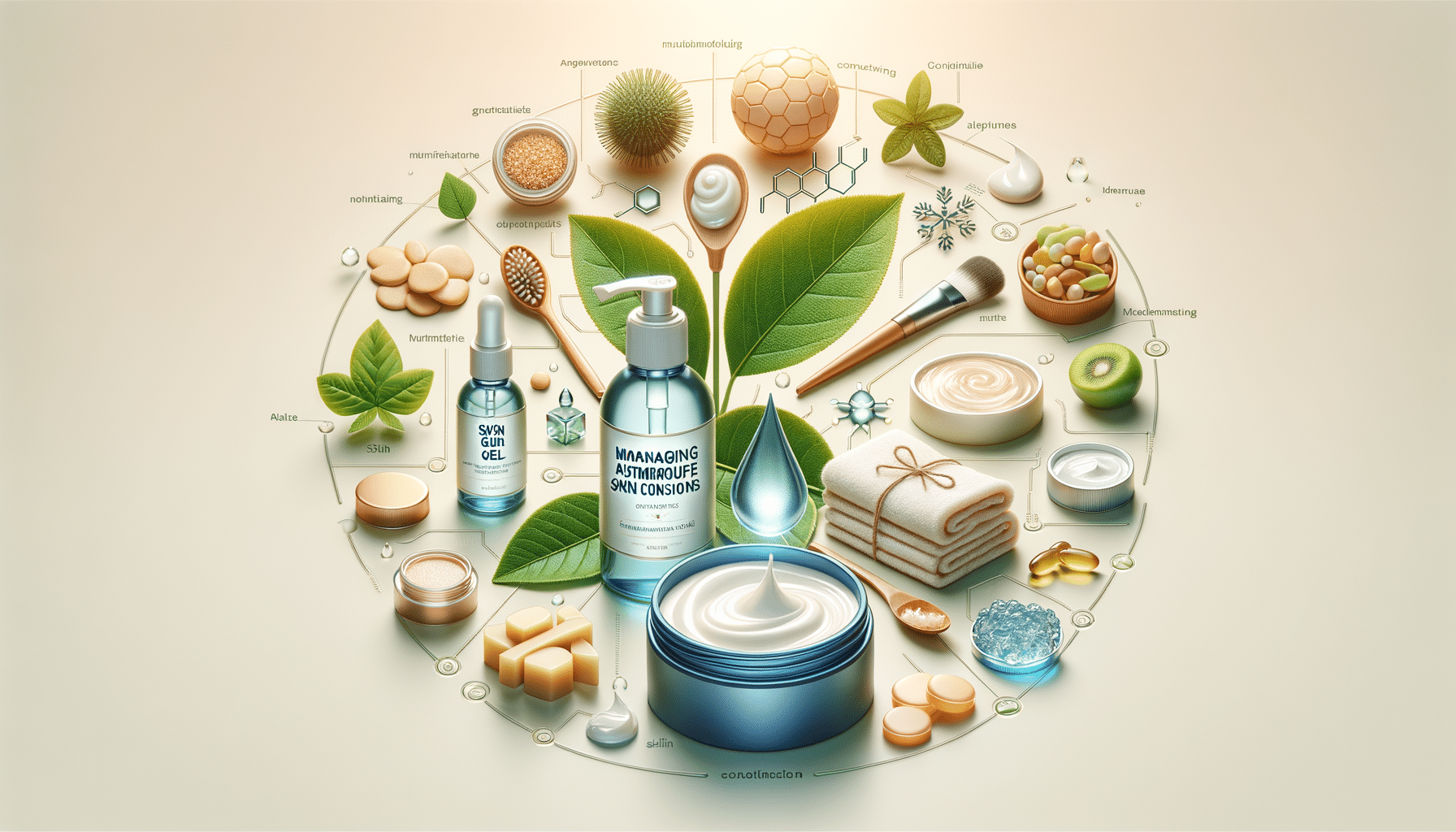
Autoimmune skin conditions represent a complex intersection of dermatology and immunology, where the body’s own immune system mistakenly targets and attacks healthy skin cells. These conditions can manifest in various forms, each with unique symptoms and challenges. Understanding these conditions is crucial for effective management and improving the quality of life for those affected. This article delves into the intricacies of autoimmune skin conditions, exploring symptoms, treatment options, and strategies for managing flare-ups.
Common Autoimmune Skin Conditions
Several autoimmune skin conditions are prevalent, each with distinct characteristics. Psoriasis, for instance, is characterized by red, scaly patches that can be itchy and painful. Vitiligo, on the other hand, leads to the loss of skin pigment, resulting in white patches. Another condition, lupus, can cause a butterfly-shaped rash across the face. These conditions not only affect the skin but can also have systemic implications, impacting joints and other organs.
While the exact cause of these conditions remains elusive, genetic predisposition and environmental factors are believed to play a significant role. Understanding the specific condition is essential for tailoring treatment and management strategies, which often involve a combination of topical treatments, systemic medications, and lifestyle modifications.
Symptoms and Diagnosis
Symptoms of autoimmune skin conditions can vary widely depending on the specific disorder. Common symptoms include redness, swelling, itchiness, and the formation of blisters or lesions. In some cases, symptoms may extend beyond the skin, affecting other parts of the body such as joints or internal organs.
Diagnosing these conditions typically involves a comprehensive approach, including a detailed medical history, physical examination, and laboratory tests. Skin biopsies may also be conducted to confirm the diagnosis. Early and accurate diagnosis is crucial for effective treatment, as it allows for the implementation of targeted therapies that can help manage symptoms and prevent complications.
Treatment Options
Treatment for autoimmune skin conditions is often multifaceted, aiming to reduce symptoms and control flare-ups. Topical treatments, such as corticosteroids and calcineurin inhibitors, are commonly used to manage inflammation and irritation. Systemic treatments, including immunosuppressants and biologics, may be prescribed for more severe cases.
In addition to medical treatments, lifestyle modifications can play a significant role in managing these conditions. Stress management, a balanced diet, and avoiding known triggers are essential components of a comprehensive treatment plan. Regular follow-ups with healthcare providers are also important to monitor the condition and adjust treatments as needed.
Managing Flare-Ups
Flare-ups are common with autoimmune skin conditions and can be triggered by various factors, including stress, infections, and environmental changes. Effective management of flare-ups involves a proactive approach, incorporating both preventative and responsive strategies.
Preventative measures include maintaining a consistent skincare routine, using gentle, non-irritating products, and protecting the skin from harsh environmental conditions. During a flare-up, it is important to adhere to prescribed treatments and avoid potential irritants. Support from healthcare providers, along with patient education, can empower individuals to manage their condition effectively and reduce the impact of flare-ups on their daily lives.