Managing the Flare-Ups
Understanding Autoimmune Skin Conditions
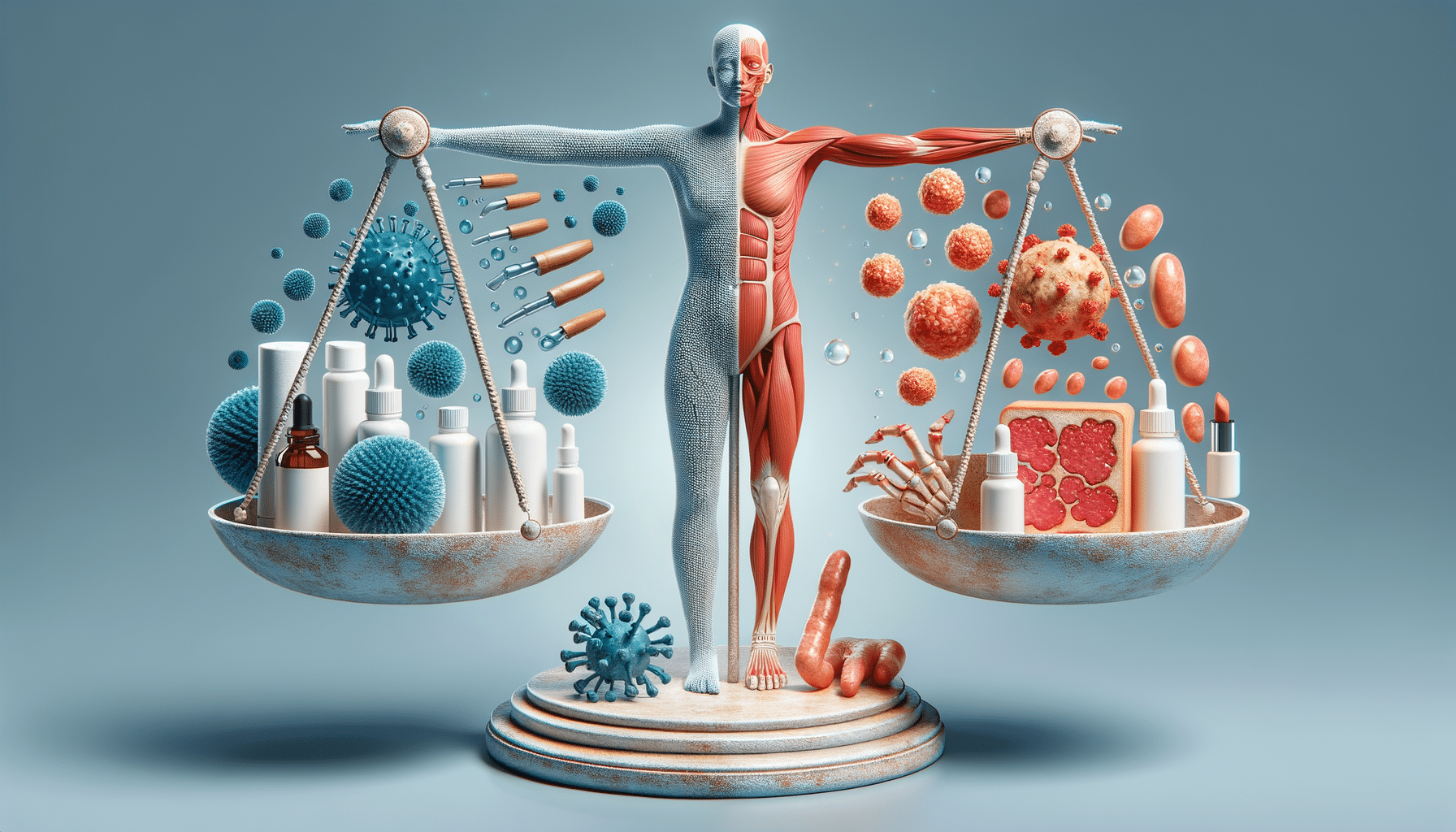
Autoimmune skin conditions are a group of disorders where the immune system mistakenly attacks healthy skin cells. This can lead to a range of symptoms, including redness, swelling, blisters, and intense itching. These conditions are often chronic, meaning they can persist for a long time or recur frequently. Understanding the underlying mechanisms of these conditions is essential for effective management.
Some common autoimmune skin conditions include psoriasis, lupus, and vitiligo. Each of these conditions has unique characteristics and symptoms, but they all share the common feature of being driven by an overactive immune response. For example, psoriasis is characterized by the rapid growth of skin cells, leading to thick, scaly patches. Lupus can cause a butterfly-shaped rash on the face, among other systemic symptoms, while vitiligo leads to the loss of skin pigmentation.
Diagnosis of autoimmune skin conditions typically involves a combination of physical examination, medical history, and laboratory tests. Dermatologists may perform skin biopsies or blood tests to identify specific antibodies or markers associated with these disorders. Early diagnosis is crucial for managing symptoms and preventing complications.
Symptoms and Triggers
The symptoms of autoimmune skin conditions can vary widely depending on the specific disorder. Common symptoms include:
- Red, inflamed patches of skin
- Blisters or sores that may ooze or crust over
- Changes in skin color or texture
- Intense itching or burning sensations
- Thickened, scaly skin
Identifying triggers that exacerbate these symptoms is a key part of managing autoimmune skin conditions. Common triggers include stress, infections, certain medications, and environmental factors like extreme temperatures or sunlight exposure. Keeping a symptom diary can help individuals identify patterns and pinpoint specific triggers, allowing for better management of flare-ups.
It is also important to differentiate between symptoms caused by the autoimmune disorder itself and those resulting from secondary infections or other complications. Consulting a healthcare professional can provide clarity and ensure appropriate treatment.
Treatment Options
Treatment for autoimmune skin conditions often involves a combination of lifestyle changes, medications, and therapies aimed at reducing symptoms and preventing flare-ups. The choice of treatment depends on the specific condition and its severity.
Common treatment options include:
- Topical treatments: Creams and ointments that reduce inflammation and soothe irritated skin.
- Systemic medications: Oral or injectable medications that suppress the immune system to prevent it from attacking healthy skin cells.
- Light therapy: Controlled exposure to ultraviolet light can help reduce symptoms in certain conditions like psoriasis.
- Dietary changes: Some individuals find relief by avoiding specific foods that trigger symptoms.
In addition to these treatments, stress management techniques such as meditation, yoga, or counseling can be beneficial, as stress is a known trigger for many autoimmune conditions. Working closely with a healthcare provider to tailor a personalized treatment plan is essential for effective management.
Lifestyle and Coping Strategies
Living with an autoimmune skin condition can be challenging, but adopting certain lifestyle and coping strategies can significantly improve quality of life. Here are some tips to consider:
- Maintain a regular skincare routine to keep skin moisturized and protected from irritants.
- Wear sun-protective clothing and apply sunscreen to prevent sun-induced flare-ups.
- Practice stress-reduction techniques such as mindfulness, deep breathing exercises, and regular physical activity.
- Join support groups or online communities to connect with others who share similar experiences and challenges.
It is also important to educate family and friends about the condition to foster understanding and support. Open communication with healthcare providers can help address any concerns and ensure that treatment plans are effective and tailored to individual needs.
Conclusion: Navigating Life with Autoimmune Skin Conditions
Autoimmune skin conditions can be a source of discomfort and frustration, but with the right approach, individuals can manage their symptoms and lead fulfilling lives. Understanding the nature of these conditions, recognizing triggers, and adhering to personalized treatment plans are crucial steps in managing flare-ups and improving overall well-being.
By staying informed and proactive, individuals can navigate the complexities of autoimmune skin conditions with confidence and resilience. Ongoing research continues to shed light on these disorders, offering hope for more effective treatments and potential cures in the future.