Managing the Flare-Ups
Understanding Autoimmune Skin Conditions
Autoimmune skin conditions are a group of disorders where the immune system mistakenly attacks healthy skin cells, leading to inflammation and various skin issues. These conditions can manifest in numerous ways, ranging from mild rashes to severe blistering and lesions. The impact on a person’s quality of life can be significant, affecting not only physical health but also emotional well-being. Understanding the underlying mechanisms of these conditions is crucial for effective management and treatment.
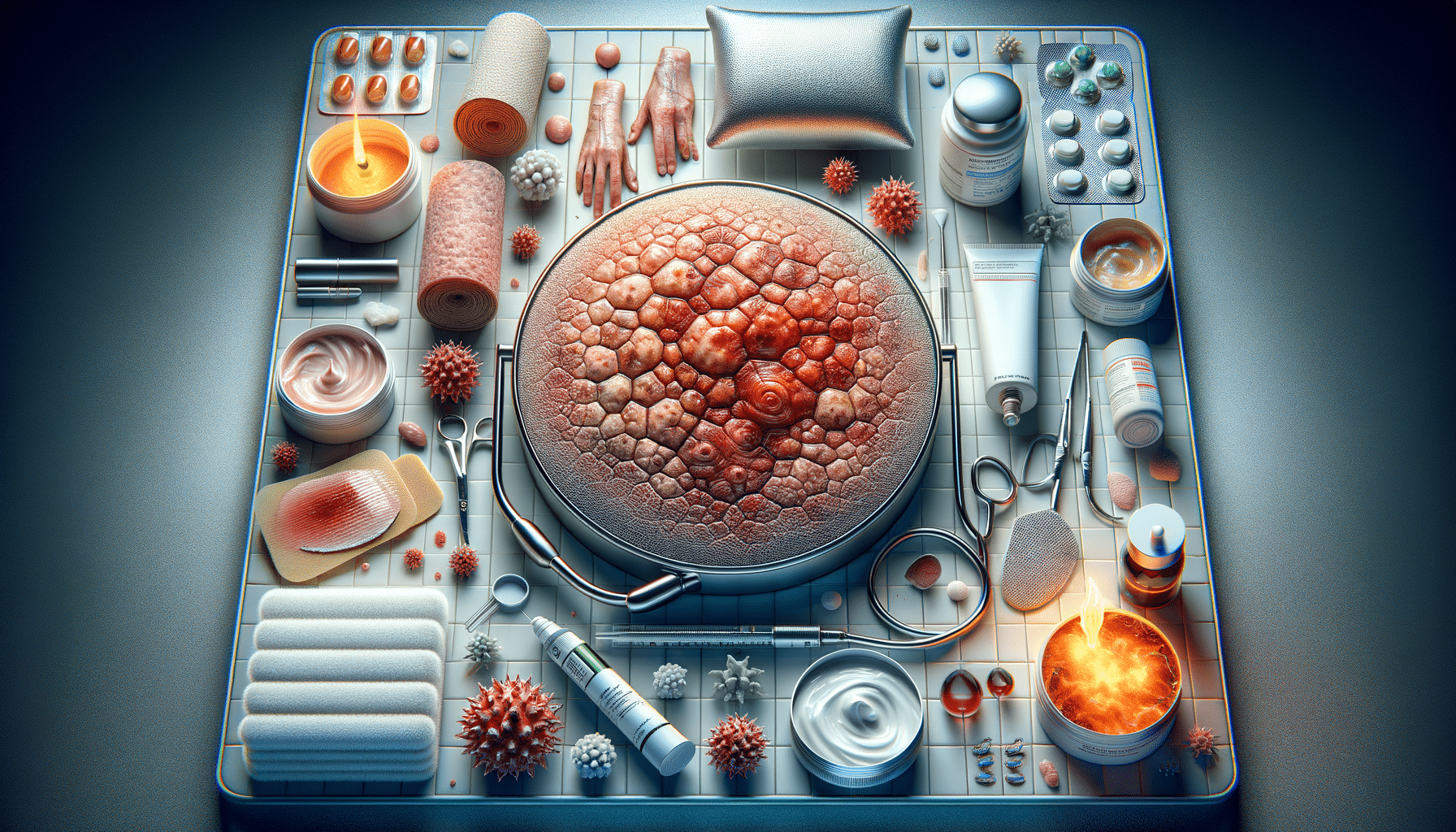
Common autoimmune skin conditions include psoriasis, lupus, and vitiligo, each with its unique set of symptoms and triggers. For instance, psoriasis is characterized by red, scaly patches on the skin, while lupus can cause a butterfly-shaped rash across the face. Vitiligo, on the other hand, leads to the loss of skin pigment, resulting in white patches. These conditions are chronic, meaning they persist over a long period and can have periods of remission and flare-ups.
Diagnosis often involves a combination of physical examination, medical history, and specialized tests such as skin biopsies or blood tests. Early detection and intervention are key to managing symptoms and preventing complications. While there is no cure for autoimmune skin conditions, various treatments can help control symptoms and improve quality of life.
Identifying Symptoms and Triggers
Recognizing the symptoms of autoimmune skin conditions is the first step towards effective management. Symptoms can vary widely but often include redness, swelling, itching, and pain. In some cases, blisters or lesions may form, which can be particularly distressing. It’s important to note that symptoms can fluctuate, with periods of exacerbation known as flare-ups.
Identifying triggers is equally important in managing these conditions. Triggers can include stress, certain foods, environmental factors, and even weather changes. Keeping a symptom diary can be a helpful tool for identifying patterns and potential triggers. This information can then be used to develop a personalized management plan in collaboration with healthcare professionals.
Some common triggers for autoimmune skin conditions include:
- Stress and emotional upheaval
- Exposure to sunlight or ultraviolet light
- Infections or illnesses
- Hormonal changes
- Certain medications
By understanding and avoiding triggers, individuals can reduce the frequency and severity of flare-ups, leading to better overall management of their condition.
Treatment Options and Therapies
Treatment for autoimmune skin conditions is highly individualized, focusing on alleviating symptoms and preventing flare-ups. The choice of treatment depends on the specific condition, its severity, and the patient’s overall health. Common treatment options include topical treatments, systemic medications, and lifestyle modifications.
Topical treatments, such as corticosteroids and immunomodulators, are often used to reduce inflammation and suppress the immune response. These are applied directly to the affected skin areas and can provide relief from symptoms like itching and redness. For more severe cases, systemic medications, including immunosuppressants and biologics, may be prescribed. These medications work throughout the body to control the immune system’s activity.
In addition to medical treatments, lifestyle modifications can play a crucial role in managing autoimmune skin conditions. This may involve adopting a healthy diet, managing stress through techniques like meditation or yoga, and protecting the skin from potential irritants. Regular follow-ups with a dermatologist or healthcare provider are essential to monitor the condition and adjust treatments as needed.
Living with Autoimmune Skin Conditions
Living with an autoimmune skin condition can be challenging, but with the right strategies, individuals can lead fulfilling lives. Education and awareness are key components in managing these conditions effectively. By understanding the nature of their condition, individuals can make informed decisions about their treatment and lifestyle choices.
Support groups and online communities can provide valuable resources and emotional support. Sharing experiences with others who have similar conditions can offer comfort and practical advice. Additionally, staying informed about new research and treatment options can empower individuals to advocate for their health needs.
It’s also important to maintain a positive outlook and focus on self-care. Engaging in activities that promote relaxation and well-being can help manage stress, which is a common trigger for flare-ups. By taking a proactive approach, individuals can minimize the impact of their condition on daily life and enhance their overall quality of life.
Conclusion: Navigating the Path to Relief
Autoimmune skin conditions present unique challenges, but with the right approach, individuals can manage symptoms and improve their quality of life. Understanding the nature of these conditions, identifying triggers, and exploring various treatment options are essential steps in this journey. By staying informed and proactive, individuals can navigate the complexities of their condition and find relief.
While there may be no cure, advancements in medical research continue to offer hope for more effective treatments in the future. By fostering a supportive environment and focusing on self-care, individuals can minimize the impact of autoimmune skin conditions and embrace a healthier, more fulfilling life.